“We’re using yesterday’s technology for the biggest public health emergency in our lifetimes. COVID-19 has demonstrated for people what we’ve known all along. You can’t leave public health at the end of the line,” Janet Hamilton, executive director of the Council of State and Territorial Epidemiologists is quoted as saying in a recent Fortune article.
Astonishing Gaps in Digital Transformation
I said I was finished writing about the pandemic. But the crisis continues to expose astonishing gaps in digital transformation at the highest levels. As DX experts, we are bound to recommend solutions where possible.
Here is the mission-critical Coronavirus Case Report form issued by the Centers for Disease Control (CDC) located in Atlanta, Georgia. The CDC has a strategic initiative underway to replace paper and fax forms with an electronic data reporting system and has made good progress in many areas. So then, one would assume something this urgent and critical could be completed online, and the data immediately available for analysis and action.
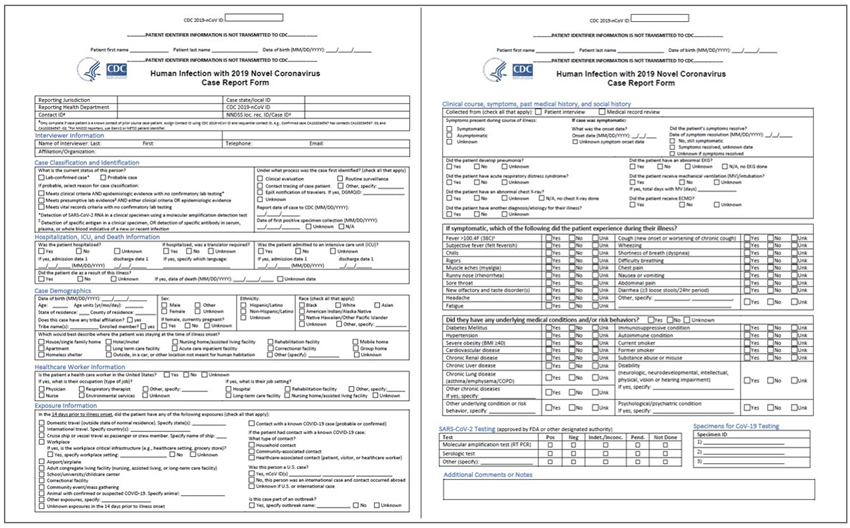
However, the Coronavirus Case Report is a PDF downloaded from the CDC website.1 It is not a “computer fill-in form” so it must be printed out and completed by hand.
The form is complex and could take an interviewer at least 30 minutes to complete. At some later point in time that varies from hospital to hospital, the form is faxed to the CDC. There, workers must decipher the handwriting and enter data into a central database that can be shared with public health departments across the United States who desperately need to analyze this information for forecasts and public health guidelines.
Meanwhile in Texas
A surge of new cases has emerged in Texas after the state re-opened, and worried state officials are trying to ramp up contact tracing efforts. In an NBC News story, a health official revealed this week that information about hundreds of new cases is pouring in daily across the state, submitted not online or through email, but via fax.
Dr. Mark Escott, the interim medical director and health authority for Austin Public Health, reported that “sometimes those faxes are positives and sometimes they’re negatives. Sometimes they have information like the person’s phone number that was tested and sometimes they don’t. So we have a whole team of people who have to sort through more than a thousand faxes a day to sort out the positives versus the negatives.”
In the same story, Lauren Ancel Meyers, a professor of integrative biology who leads the COVID-19 Modeling Consortium at the University of Texas at Austin, said while state-of-the art tracking and tracing technology would be helpful, it “just doesn’t exist because we never had a need for it before.”
Why Fight a 21st Century Pandemic with 19th Century Information Tools?
The states all want to reopen for business as soon as safe and feasible. This depends on making current and accurate medical data about the spread and tendencies of the virus available to public health officials. Hospitals are collecting this data into their electronic health records (EHR) systems.
But because hospitals use incompatible proprietary EHR software, electronic health records often must be printed out first, faxed and then re-entered by public health authorities. This outdated process is wasting valuable time and leading to potentially harmful transcription errors.
The first fax was sent in the 19th century. Fax was long ago replaced by other secure and efficient document and data transmission technologies. The healthcare industry has been too slow to upgrade.
Forms faxed between hospitals and laboratories often are missing critical information, leading to delays in contacting patients and identifying the people with whom they had close contact. In the same Fortune article, Hamilton went on to say, “In some states, demographic information on race and ethnicity is missing 85% of the time, and patients’ addresses (are missing) half the time.”3
Is this any way to run a pandemic response effort?
Atlanta, We Have a Solution
We get it, CDC. Nothing in this world is more mission-critical than patient treatment, so you do need to be cautious. Therefore, the data collection process must be demonstrably accurate and must be predictable across disparate sources.
Companies such as Parascript who make Intelligent Document Processing (IDP) software have proven their value and integrity in automating the data collection from healthcare forms like the Coronavirus Case Report Form. IDP software can provide a cost-effective ability to access this data to support efforts all over the U.S. to increase the standard of care and improve outcomes while, at the same time, reducing costs.
Finding the Needle in the Haystack
Medical charts represent a treasure trove of unstructured data that could help in the fight. The images can be parsed and analyzed using IDP in order to identify hidden patterns. While EHR/EMR-based data is available (though as shown above, it is hard to collect), much useful qualitative data is stored within the complex structure of medical charts, each made-up of different medical records that rarely have needed data which is uniformly located in the same position.

Parascript Software Can Also Read Handwriting
Additionally, analysis of data in medical charts requires treating each medical record as a separate entity. However, many charts exist as single monolithic PDF files containing many discrete records. So not only is there a challenge with accessing data from each record, but there is the challenge of separating each chart file into individual records.
Where Machine Learning Really Makes a Difference
Using machine learning algorithms, IDP software can be trained on medical charts to identify key characteristics of each individual medical record. Different algorithms are often employed that evaluate various attributes such as presence of graphical information (e.g., logos), textual data (e.g., facility names and addresses), and even spatial information such as the distance between different dates on a page, and use of specific language related to those dates.
All these attributes are then analyzed to identify the most reliable way to identify and separate one record from another. Once separated, data extraction can then be employed with the final step being to employ IDP to further identify specific patterns in the text that can reveal various problems and conditions not only with a single patient, but across a patient population.
Conclusion
Clearly, this technology should be deployed immediately to assist with COVID-19 data collection. If you are tasked to collect data from printed and faxed forms or PDF documents, now is the time to consult an expert who can evaluate your current system and help you accelerate the time to a 21st century solution.
Footnotes
1 https://www.cdc.gov/coronavirus/2019-ncov/downloads/pui-form.pdf
Digital Insurance recently hosted the Insurance Optimized for Cost, But at Risk for Disruption webinar with BRYJ and Parascript (the sponsor) that specifically focuses on intelligent capture within the insurance industry.



