Today, healthcare is a multi-trillion-dollar business in the United States. According to the U.S. Centers for Medicare & Medicaid Services, in 2018 US healthcare spending reached $3.6 trillion, or $11,172 per person. That’s almost 18% of the nation’s Gross Domestic Product.
Even more staggering is the number of medical billing errors that occur each year in the United States. Experts say that between 30% and 80% of medical bills contain errors. While doctors and hospitals in the U.S. leave billions of dollars on the table each year due to poor billing practices, it’s the patients who are suffering the most.
A study by NerdWallet found that medical debt is the single largest category of consumer debt in the US. One in six Americans will have a medical bill turned over to a debt collection agency. Another recent study from academic researchers found that 66.5% of all bankruptcies were tied to medical issues — either because of high costs for care or time out of work. An estimated 530,000 families turn to bankruptcy each year because of medical issues and bills, the research found.
Healthcare claims processing is clearly an area that is ripe for improvement.
Americans can barely afford their health care as it is. We certainly can’t afford to overpay due to claims processing errors. Healthcare claims processing is clearly an area that is ripe for improvement. With the huge size of expenditures and crushing costs inflicted on patients, even a small, incremental improvement in data processing accuracy could result in hundreds of millions of dollars in savings for everyone involved.
Why is Processing Healthcare Claims Still an Issue?
Good progress has been made over the past ten years, as more medical claims are handled through a process called auto-adjudication. This is the ability of computers to accept electronically generated claims forms (EDI) and automate the processing using a rules engine. Approximately 90% of claims now go through this process.
However, there remain two classes of claims that stubbornly elude all attempts to process through auto-adjudication. The first type is submitted on forms that are scanned, mailed or even still faxed between medical providers and the insurance companies. The second type are those claims that cannot be resolved on the first pass and require the submission of additional supporting documentation. Both classes require a different approach to automation, using advanced computer vision along with machine learning.
Both classes are also responsible for an outsized amount of the overall costs of claims processing and for an equally outsized percentage of all errors. This is because they have traditionally been handled by human beings who perform manual processes that include receiving and separating the claims into discrete service encounters, entering the data into the processing system, and collating any supporting documentation.
As with any manual document process, the errors and delays can be drastically reduced by the application of new machine learning software and intelligent document processing technologies.
Advances in Machine Learning Can Help Close the Gap
With the advent of machine learning, it is now possible to train a system to emulate the actions of human workers in order to automate a high percentage of typical work, including intake of documents, sorting and verifying that the required data is present, and entering that data in various systems. Even work that is not routine or that requires more sophisticated analysis can be made more efficient.
If you are looking to improve your own processing of these difficult to handle claims types, here are the key functions to look for in a software solution.
- Superior automation for black-and-white forms. Black-and-white claims forms can be converted to simulate drop-out ink forms; images are analyzed, and those that vary in size are reformatted to conform to expected layouts. When claims are copied or faxed, the software must be able to separate the pre-printed form from the actual field values.
- Handle forms of all shapes and sizes with equal ease. Non-linear, line-by-line analysis of each incoming claim in order to properly identify and align the images to pre-built fields means that scaling or distortion challenges are no longer an issue. One should also be able to process both drop-out and black-and-white images in the same workflow.
- Taking advantage of unparalleled built-in accuracy. Should provide not only pre-built configuration for claims forms, but also provide that each field is tuned and optimized to achieve a specific statistically measured accuracy rate. This choice allows you to select the accuracy that you require to completely remove human verification for a portion of your data processing.
- Handwriting extraction. The ability to extract data from handwriting from standard CMS forms as well as non-standard attachments.
- Out-of-the-box support for CMS-1500 and CMS-1450 Forms. Must have support for the location and extraction of all fields contained on the standard CMS-1500 and CMS-1450 forms in a single input stream with guaranteed field-level accuracy. This means less time configuring and more time processing.
- Field-level OCR. This provides superior throughput performance compared to full-page OCR. The result is that you can process more claims in a smaller amount of time with greater accuracy.
- Higher accuracy to comply with SLAs. Built-in support for validation of CPT and ICD-10 data, bringing the higher accuracy needed to support stringent data quality SLAs.
- Protect PHI. Must have data validation workflows that support field-level review so that no single user has a complete view of Patient Health Information (PHI).
- Auto-classification of forms. Automated classification of claims and supporting documents reduces the need for manual batch preparation and routing.
Handling Even the Most Difficult Forms
Some claims forms will require additional processing, especially those submitted via fax which is still common throughout the medical profession. Parascript has developed Virtual Drop-out, a technology powered by deep learning neural networks. Poor-quality, faxed CMS1450 and 1500 forms are analyzed and perfected to the quality of a drop-out ink form, leaving only the data and eliminating the underlying form structure.
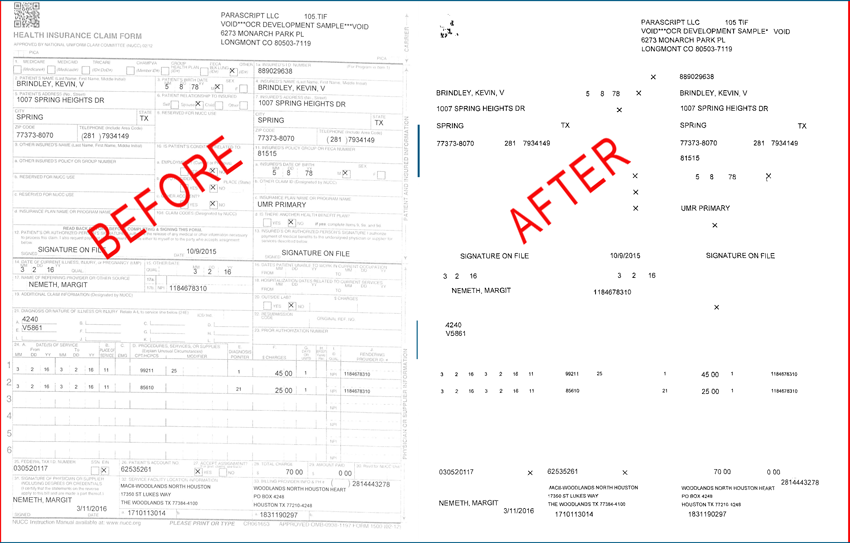
Parascript’s ground-breaking Virtual Drop-out technology is the most accurate for black-and-white (B&W) medical forms such as this.
For claims accompanied by handwritten correspondence, Parascript has perfected advanced handwriting recognizers that can automatically transcribe the information into machine-readable data and then apply the latest text analysis to aid with either auto-adjudication or manual review.
By harnessing the power of Parascript’s advanced automation and machine learning, the “last mile” of claims processing – that shortest yet most difficult gap – can finally be addressed.



